When Your Child Has Tuberculosis
Tuberculosis (TB) is a disease caused by bacteria (germs) that can spread from person to person. It's carried through the air in tiny droplets. Most often, TB infects the lungs, but it also can harm other parts of the body. When not treated properly, TB can be fatal. There are two types of TB: latent (inactive) and active. Most children who have TB have the latent form.
Inactive (latent) TB
If your child has been diagnosed with latent TB, it means your child:
-
Has live TB bacteria in the lungs, but the germs have been sealed off, much like a scab covers a wound. As a result, your child doesn’t have symptoms or feel sick. The only way to know your child has latent TB is with a TB test.
-
Can’t spread the infection to others.
-
Will need medicine to prevent the infection from becoming active at a later time.
Active TB
If your child has been diagnosed with active TB, it means your child:
-
Has active infection causing symptoms from TB, such as a lasting cough, phlegm, extreme tiredness (fatigue), fever, night sweats, or weight loss. Your child is likely to feel very sick.
-
Can spread the infection to others if the active TB involves the lung or throat.
-
Must take medicine to help cure the disease.
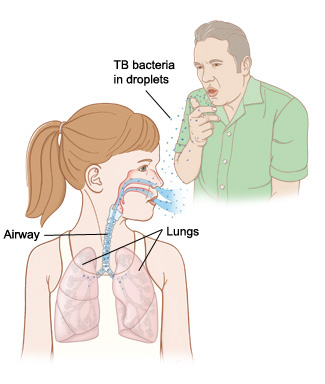
How does TB spread?
TB bacteria are released into the air in tiny droplets when someone with active TB disease of the lungs or throat coughs, sneezes, or talks. The germs spread easily, especially in crowded spaces with poor airflow. Children who have close contact with someone with active TB and breathe in the germs for weeks or more are likely to become infected. Children are at special risk of TB if they:
-
Spend time every day with someone who has active TB.
-
Live in a crowded place, such as a shelter or group home, where germs spread easily.
-
Travel to or come from a country where TB is common.
-
Have a weak immune system or have HIV infection.
What are the symptoms of TB?
In children, symptoms may include:
-
Fever
-
Fatigue or weakness
-
Weight loss
-
Night sweats
-
Weakness
-
Irritability
-
Enlarged glands
Symptoms of TB infection in the lungs include:
How is TB diagnosed?
There are 2 tests that can help detect latent TB infection:
-
Skin test (PPD). A testing solution is placed just beneath the skin on your child’s arm to see if a reaction (such as a hard, red bump) occurs. Your child will need to return to the office in 2 or 3 days to have the arm checked. Be sure to keep the appointment. You will learn the test results during this visit.
-
Blood test. In this test, a small amount of blood is drawn and sent to a lab for testing. Your doctor can tell you whether this test is right for your child.
For active TB disease, samples are taken from the involved area of the body (such as sputum, pus, or a biopsy) and testing is done on the samples to see if there is active TB infection.
What do the test results mean?
-
A negative skin or blood TB test usually means that your child’s body is free of TB bacteria.
-
A positive result means your child has likely been exposed to the germs that cause TB. Other tests, such as a chest X-ray, are needed to learn whether the infection is active. Your child’s healthcare provider may also take a sample of your child’s stomach secretions or mucus that comes up when your child coughs (sputum). These samples are sent to a lab and tested for TB bacteria. This helps the provider choose the best medicine for your child.
How is TB treated?
Both latent and active TB are treated with antibiotic medicines. Children with active TB take more antibiotics and for a longer time. Your child should begin feeling better shortly after starting treatment. But your child must continue to take all the medicine prescribed. This is the only way to cure the disease. Not taking all the medicine means your child won’t get well and can keep spreading the disease to others.
What is DOT?
During treatment, your child may be offered or required to participate in a program called DOT (directly observed therapy). In this program, a nurse or healthcare worker gives the medicine to your child and watches them take it. DOT has been shown to result in better cure rates in people with active TB and is especially important with infectious forms of active TB such as when there is lung infection.
Caring for your child at home
To help your child recover fully from active TB or to treat latent TB:
-
Make sure your child takes all the medicine as directed, even when symptoms improve. Your child will take the medicine for 4 to 6 months or longer. Sticking to this schedule takes patience. But stopping medicine early or skipping doses means your child won’t get well. And it can create TB germs that are more deadly and harder to treat.
-
Arrange for your child to sleep in a room with good airflow.
-
Be sure your child gets plenty of rest and eats healthy meals. A nutritious diet full of fresh fruits and vegetables helps the body fight infection.
-
Check with your child’s healthcare provider before using any prescription or over-the-counter medicines that haven’t been prescribed. Don’t give your child cough syrup. It won’t help and may be harmful.
Follow-up care
Be sure your child goes to all follow-up exams. These help ensure that the medicine is working, that side effects are being monitored and treated, and that your child's form of TB is getting better.
Preventing the spread of active TB
To help keep others safe when your child has active TB involving the lungs or throat:
-
Ask family, friends, and anyone else in close contact with your child to get tested. If your child has active TB, the TB germs can spread to other people.
-
Teach children to wash their hands often, particularly after coughing.
-
Make sure your child coughs into a tissue.
-
Use a plastic bag to throw away used tissues and other supplies.
When to call your child's healthcare provider
Call the healthcare provider if your child: